By Dr Fiona McMillan
Let’s begin with a remarkable fact. Right now there are ten times as many microorganisms (‘microbes’) in and on your body than there are human cells. In effect, most of you is not actually you. It’s a sobering thought, but no cause for alarm according to Professor Mark Morrison, Chair of Microbial Biology and Metagenomics at the University of Queensland Diamantina Institute (UQDI). In fact, it’s to be expected.
“We live in a microbial world,” he explains. “From polar ice caps to the deepest thermal vents. We’re surrounded by microorganisms and they provide a variety of goods and services. Why should the human body be any different to any other part of the planet in terms of serving as a portal for the microbial world?”
Indeed, we make very good hosts for microbes. Think you know the back of your hand? Any single square centimetre on the surface of your skin is home to more than 4 million microbes. The gastrointestinal tract presents an even larger place for microbes to call home, providing approximately 30 square metres of direct interface with the human body. Morrison likens it to an inland sea, where in any given teaspoon you can find 10 billion microbes. Some of these we know quite well, but others are still aliens. The more we understand about them, the more we learn about our own health.
We now know that gut microbes have a profound effect on the development of our immune systems, and influence our susceptibility to immune-related diseases. Morrison gives two compelling examples. If you take two genetically identical mice, both pre-disposed to the mouse version of rheumatoid arthritis, and raise them in a sterile, microbe-free environment, they stay healthy. But if one is transferred to a normal environment full of microbes, it will develop the autoimmune disease.
“We see that a genetic change, coupled with the microbiota leads to a strong immune effect,” says Morrison. In other words, genetics play an important role in autoimmune disease, but microbes are also required.
Yet Morrison is quick to add, “They can also keep you well.”
Let’s look at another pair of mice: one is genetically prone to autoimmune disease and one is a normal ‘control’ mouse. If they are raised separately in non-sterile conditions, the genetically prone mouse will develop the autoimmune disease, while the control mouse will not. But if they are then placed in the same cage, the symptoms of the first mouse will improve as it picks up bacteria from the healthy mouse.
It is becoming clear that your health is influenced by a complex interplay between your genes, your immune system, your diet, your environment, and a staggering diversity of microbes. This raises an interesting prospect: can we find out precisely which microbes drive or mitigate which diseases, and how?
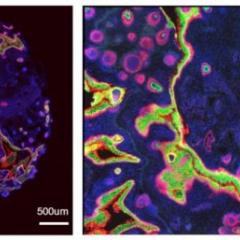
To do this we need a better understanding of human gut microbes, and at 10 billion a teaspoon, this is no simple task. That’s why Morrison is excited about metagenomics, because it allows him to extract a great deal of information from very small samples. Using cutting edge sequencing technology at UQDI he and his colleagues are able isolate fragments of microbe DNA from a sample of gut tissue. These fragments are like genetic fingerprints that reveal which genes are present in the microbiota; this in turn reveals which microbes are there and what their relative abundances are. Morrison and his colleagues are also able to rapidly sequence entire genomes of individual microbes. By also collaborating with mathematicians and statisticians, they can visualise the differences between microbial communities.
For Morrison, the advantages of metagenomics are substantial. “It enables better understanding of the full genetic potential that resides in the microbial community.” In essence, he adds, “we’re building a blue print of how these organisms work.”
His group is currently using this approach to profile the gut microbiota of Inflammatory Bowel Disease (IBD) patients. He is optimistic that this work will yield clinical benefits, particularly given recent findings by Spanish and French colleagues, as well as collaborations with leading IBD clinicians here in Australia. Their profiling of gut microbiota in ulcerative colitis (UC) and Crohn’s
Disease has revealed particular species of bacteria that reduce inflammation and help restore a healthy gut. These initial clinical trials show that these bacteria are measurable and persistent in those patients who also demonstrate better health outcomes.
Morrison adds that you don’t need to be genetically predisposed to an immune disease for your health to be substantially affected by your gut microbes. They play a role in a wide range of human conditions, including cardiovascular conditions, susceptibility to certain viral infections, and obesity.
When you transfer the microbiota from a lean human to a mouse, and also transfer the microbiota from that person’s obese twin to another mouse, each mouse develops the same phenotype as the donor, becoming either lean or obese, respectively. If you bring these mice together and then feed them a low fat diet, not only does the obese mouse lose weight, but it also “receives” gut microbes from the lean mouse. It has also been shown that when bacteria from a morbidly obese human is introduced into the gut of a germ-free mouse, the mouse similarly becomes obese and develops insulin resistance, but only when given a high fat diet. These studies are part of a growing body of evidence that demonstrates how microbes and diet together influence our health and well-being.
But it doesn’t stop there. Microbes appear to influence the way we age, and vice versa.
“Our microbial world ages with us,” says Morrison. “There are influences from pregnancy and child birth, as well as the choices mothers make during infancy through to toddler age. Once we get to around age 3 or 4 the microbial community is rather stable.” After this point, he explains, environmental influences have a stronger effect, even over and above genetics; this in turn holds sway over health.
The ultimate goal is to define a “healthy microbiota” in terms of the functional benefits it can provide, and to also determine what variety of gut microbes works best for any one individual. This information could be used to maintain good health or improve poor health through diet and perhaps also through the development of microbe based treatments. More research is needed to meet that goal, but Morrison believes it’s certainly achievable. As part of the Translational Research Institute, UQDI researchers such as Morrison are able to benefit from close collaborations across a range of research areas, and this comes with a multitude of benefits for the study of the microbiome.
“As a microbiologist, my field is being transformed by not just the quantity of the data we can produce but how rapidly we can produce it,” says Morrison. “What a place like the TRI does is provide a home for a variety of capabilities in immunology, microbiology, nutrition and metabolism, genomics and other areas where we work together with a view of trying to make a big difference to health and well-being.”
Media: Kate Templeman, +61 7 3443 7027 or 0409 916 801, k.templeman@uq.edu.au